Little Rock, Arkansas February 2023
At the start of the pandemic, Congress enacted the Families First Coronavirus Response Act (FFCRA), which included a temporary requirement that Medicaid programs keep people continuously enrolled, and, in exchange, states received enhanced federal funding. Department of Human Services, which oversees Arkansas Medicaid, has taken several steps to educate Medicaid beneficiaries and provide them with the necessary steps to reduce coverage disruptions. SHARE, Arkansas’ only statewide HIE has collaborated with Arkansas Medicaid to provide notifications to primary care providers on the potential impact of losing Medicaid Beneficiaries. SHARE leveraged its existing patient groups and existing notification services to send out targeted reports to primary care providers throughout the state.
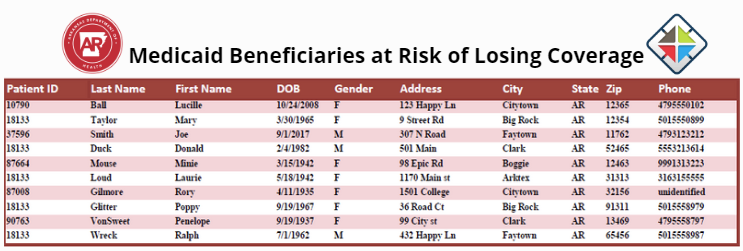
The Medicaid Beneficiaries at Risk of Losing Coverage report is a summary of a primary care physicians’ attributed Medicaid patients who are at risk of losing Medicaid coverage that has been extended due to the Public Health Emergency. Loss of coverage may impact PCCM and PCMH payments. Medicaid needs help making sure Medicaid has the most up-to-date contact information on patients who are at risk. Medicaid members can update their contact information by calling 1-800-872-2660, going to access.arkansas.gov, or by visiting their local DHS county office.
Medicaid encourages providers to visit the below site to get useful Provider tools and resources that can be shared with clients visit: https://humanservices.arkansas.gov/divisions-shared-services/medical-services/update-arkansas-2/update-arkansas-2-partner-toolkit-and-materials/


